The Health Transition Fund (HTF) comes to an end in December having scored some victories which included lowering maternal mortality rates and restoring most health facilities.
By Phyllis Mbanje
Just as it had success stories, it also had its own challenges such as the perennial tiffs over allowances which almost tore the health workforce apart. It also exposed government’s dependence on donor funding, a situation which poses questions about sustainability of projects in the absence of donor funding.

Mercy Muchero plodded on, her bulging stomach slowing her down to a waddle. As the labour pains intensified, she took one more determined step and collapsed by the roadside.
Right there in the middle of a forest somewhere in Chivi, she lay helpless and unable to stop the baby from coming.
Scared and disoriented, she pushed repeatedly, anxious to get the baby out but in the process straining and weakening the muscles of her womb (uterus) that held the baby, causing it to collapse.
Mercy is one lucky woman to have survived a collapsed womb as many women have lost their lives after failing to get medical attention.
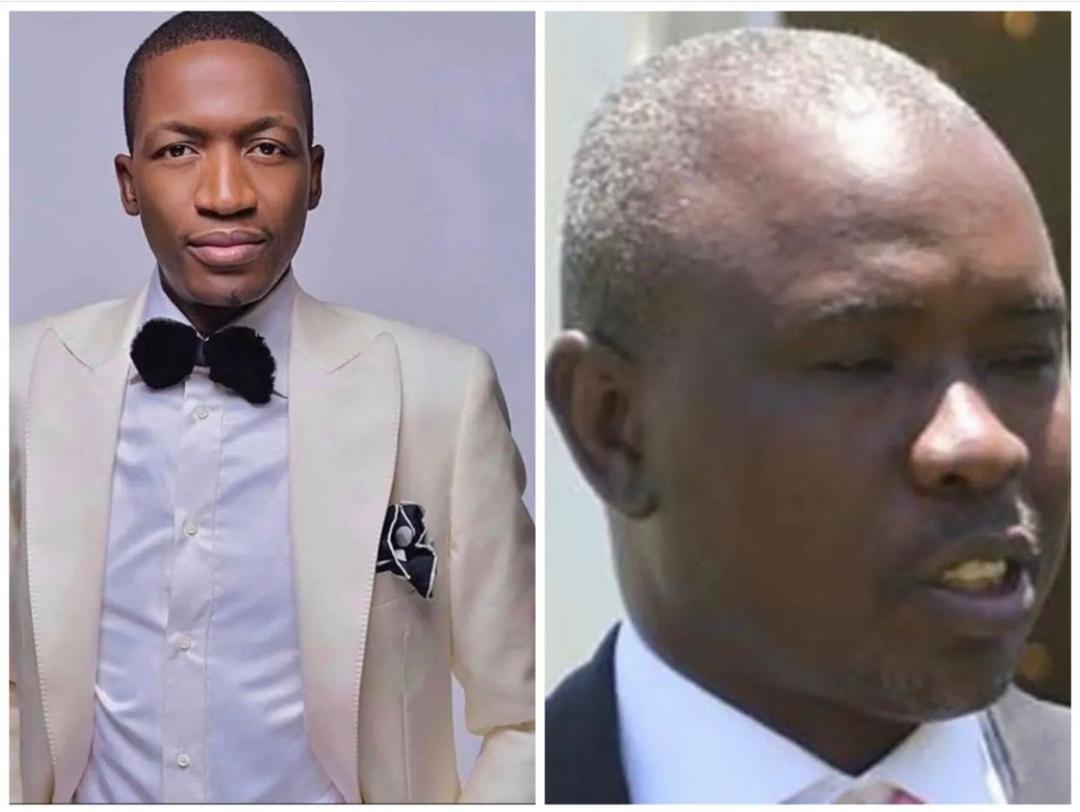
- Chamisa under fire over US$120K donation
- Mavhunga puts DeMbare into Chibuku quarterfinals
- Pension funds bet on Cabora Bassa oilfields
- Councils defy govt fire tender directive
Keep Reading
Her fate was altered by the presence of a doctor at Chivi Rural District hospital who had been recruited under the Health Transition Fund (HTF). She was able to get the necessary treatment and lived to tell her story. If however, she had come a year earlier or so when there was no single doctor at the institution, it could have been a different story.
The economic and humanitarian crisis that dogged 2008-2009 affected the health sector so badly that hospitals ceased to be places of recovery but became death traps to be avoided at all costs. Many lay in ruins with a few skeleton staff attending to patients and a meagre supply of drugs. The smell of death and disease was palpable.
Unicef representative Reza Hossaini recently proffered an honest description of the scenario, “Zimbabwe’s health sector was hemorrhaging, doctors and nurses were leaving the country in their hundreds and the few that remained were overworked and morale was very low.”
No wonder the maternal and child mortality rates were among the highest in the region. In 2002 Zimstats estimated maternal death at about 1 200 deaths per 100 000 and 94 children under five years died per 1 000 live births.

Emergency funding to Zimbabwe was dwindling and most development partners could not channel money through government.
In response to this, a multi-donor pooled fund managed by Unicef to support the health ministry was set up. The HTF was launched in 2011 and supported efforts to mobilise the necessary resources for critical interventions to revitalise the sector and increase access to care through waiving user fees for mothers and children less than five years. User fees suppressed demand for health services and pregnant women opted to deliver at home with no qualified personnel.
The fund came at a time when data showed that fewer women were attending antenatal care (ANC) which is critical in monitoring the baby and the mother.
The percentage of children between 12 and 23 who received all advised immunisations was 37%. Urgent funding support for maternal and child care was therefore required in a coordinated national scale initiative to support the health ministry.
Five donors over the years raised in total US$158 million which supported maternal, newborn and child health (MNCH) through strengthening obstetric and newborn care as well as nutrition capacity. It also purchased medical products and vaccines. Unicef serves as a common fund manager on behalf of the MOHCC.
Most rural clinics and hospitals started showing signs of recovery and according to the health minister David Parirenyatwa, even human resources vacancy rates in the institutions improved.
“We are happy to report that we have at least two doctors in each of the district hospitals in the country whereas in 2009 we hardly had any,” he said.
The minister chronicled the several positive changes that have been brought about by the fund which helped fix the health system bottlenecks in the country and saved the lives of many women like Mercy.
Through the fund, 2 500 midwives were trained and deployed and the provision of critical post allowances helped increase the number of doctors at district hospital from 70 in 2011 to 139 in 2014. But while celebrations are in order for these achievements, more so when another support the Health Development Fund (HDF) will carry on from 2016, the issue of donor dependence and over dependence has become critical.
There is growing discontent among the donors and stakeholders that the government has leaned on donor funds for too long and it is time sustainable strategies are put in place to carry forward the projects after donor aid has ceased.
The Ambassador of European Union Phillippe Van Damme recently voiced his concerns and challenged the government to increase the budget for the health sector.
An assessment of the funding system by a consultant on behalf of Unicef concluded that the HTF creates a dependency culture. An example was given of the scrapping of the user fees.
Under the HTF, pregnant women and children under five are not required to pay but now government has no money to pay for the service which should be available at every public hospital. However, most hospitals have defied the move.
“An issue in the shift however is whether government would be able to sustain the transfers should donor funding come to an end,” noted the consultant.
The issue of user fees has remained hanging with the government failing to impose the policy and now seeking a statutory instrument to enforce it.
“Our position has been very clear, pregnant women and children under the age of five should not pay user fees but the institutions are crying foul,” said the health minister in an interview.
Executive director for the Community Working Group on Health (CWGH), Itai Rusike said the current policy on user fees for maternal health needed to be supported by a legal provision in the form of a statutory instrument or an act of parliament for it to be enforceable.
“The only existing legal policy on user fees was enacted way back in the early 1980s stipulating that workers earning less than 400 Zimbabwe dollars were exempted from paying,” he said.
Currently local authorities “own” the majority of public health facilities but they do not manage all the funding and rely on government subsidies for salaries and operational costs.
Hossaini said the current dependence on external financing for no-wage expenditure was not sustainable in the long run.
“It is important that government assumes a greater share of no-wage financing because we would like to see a better prioritisation of public expenditure,” Hossaini said.
It remains to be seen if the health minister’s sentiments that they have set ambitious targets and a team to develop a new national health strategy will bear fruit.