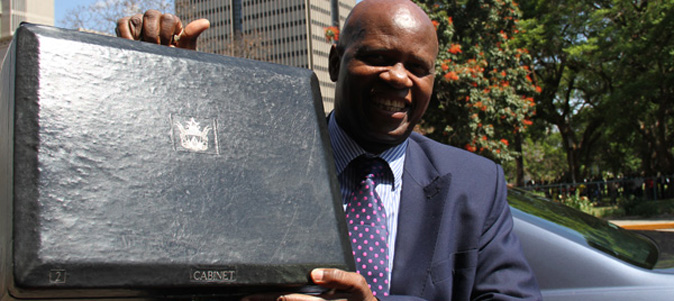
FINANCE minister Patrick Chinamasa faces a mammoth task on November 26 when he announces the 2016 national budget with increasing calls that he should give the biggest chunk of the cake to the Health ministry.
By VENERANDA LANGA
Ministry of Health and Child Care secretary Gerald Gwinji recently appeared before the Parliamentary Portfolio Committee on Health and Child Care to give his ministry’s bid for the 2016 health budget.

Gwinji told Parliament that the country was sitting on a health time bomb and did not have any choice but to give money to his ministry in this year’s budget. He revealed that Zimbabwe relied on donors for the survival of its health system and said if donors decided to pull out, the country would face a major health disaster.
“I would like to make a plea with the committee and say that we are not growing as the health sector from government resources. Any growth that we have achieved is from partner funding, and if that is withdrawn, there will be a major disaster in the country,” Gwinji said.
He said to avoid such an eventuality, the 2016 budget should allocate more resources to the health sector.
Gwinji said in 2015 the health expenditure was skewed towards employment costs, a trend which was projected to continue to next year. In 2015, salaries took up at least 90% of the total health expenditure, with capital expenditure following at only 7% and recurrent expenditure at 3%.
- Chamisa under fire over US$120K donation
- Mavhunga puts DeMbare into Chibuku quarterfinals
- Pension funds bet on Cabora Bassa oilfields
- Councils defy govt fire tender directive
Keep Reading
Community Working Group on Health (CWGH) executive director Itai Rusike told the committee that there was now need for community participation in the formulation of health budgets.
“Traditionally, the national health budget has been formulated by the technocrats at ministerial level without the direct input or suggestions from the community. Over the years CWGH has been increasingly advocating for community involvement in budget formulation as it gives a greater depth to the discussion and understanding of the health issues in the country,” Rusike said.
He said the country should strive to ensure that Chinamasa manages to allocate at least 15% of the budget towards health, in line with the Abuja Declaration.
Rusike said the current health system was such that primary health services provided by central government, church-related institutions, and others had inadequate grant support, which negatively affected provision of services.
“The resettlement of people as a result of the land reform programme placed people in remote areas which did not have health facilities and adequate sanitation, pushing them beyond the benchmark of 10km radius from a clinic. Communities in these new areas either use a lot of out-of-pocket money to travel to access care, or in a worst case scenario, decide to forgo seeking any health care services at all.”
He said the country had also struggled with a huge disease burden of tuberculosis, malaria, HIV and Aids, cholera, typhoid and other epidemic prone and non-communicable diseases, including some neglected tropical diseases. He said while some programmes were funded by donors, there were some, like the non-communicable diseases, which remained unfunded.
CWGH said about 98% of drugs in the public health system were funded by external partners, adding in the medium to long-term, over-reliance on external partner support would be counterproductive.
“Government needs to therefore increase its domestic funding as this financing mechanism has always proven to be sustainable. The existing staff establishment is not adequate to address the increasing disease burden, population and emerging health threats. For example, 23% of all provincial hospitals do not have dentists while district hospitals do not have four doctors as is required in the current establishment.”
Rusike said a significantly larger share of the budget should go to the district level to support health facilities and the first referral level. He also disclosed that only 9% of the health workers had been trained in managing injuries, trauma and other priority non-communicable diseases.
On availability of medicines in the country, Roland Mlalazi of Natpharm said the company experienced financial problems at the onset of dollarisation where they were unable to re-stock in order to supply hospitals adequately. “Some donors simply donate to the Ministry of Health [and Child Care]. The Health ministry has accumulated a $20 million debt to Natpharm, and our plea to government is for Natpharm to be capitalised so that it can go back to its mandate of procuring medicines so that it sells cheaply to hospitals,” Mlalazi said.
Vuyelwa Sidile Chitimbire of the Zimbabwe Affiliated Mission and Church Hospitals called for support of gender and youth responsive budgets in the health sector, as well as investment in health personnel, saying the current ratio of nurses to doctors and patients was very high such that it was impossible to provide efficient services.
“There is need to integrate community health workers into the system because they can actually help us to prevent other diseases. The elderly should also be supported to access health care because we have forgotten them and once we get old we will find there is no room to get treated,” Sidile Chitimbire said.
Population Services International director of medical services Edmore Munongo urged government to increase the family planning budget from 1,7% to 3%, premising his arguments on that good family planning practices had the advantages of reducing HIV incidents, as well as maternal and child mortality.
“Savings made in dealing with family planning can be diverted to investment in education and other resources for the country.”
Munongo said some of the most populous countries in the world like Nigeria and India also experienced very high maternal mortality rates, with Nigeria contributing 28% in the rate of the world’s maternal mortality.
Christopher Kamwende of the Zimbabwe Civic Society Alliance said government should consider nutrition education across the country as it was the gateway to solving a lot of health problems bedevilling people.
“In our 2014 survey, we found that 27,6% of children in the country were stunted, while 11,2% of children were under- weight and 54% of pregnant women suffered from iron deficiency. Children between 15 to 29 months are anaemic. We call on MPs to consider issues of nutrition in the budget because in 2013 only about 9,71% of the total budget was allocated to health and in 2014 it was only 8,2%, while last year it was 6,3%.
“As the budget is announced, let us also consider nutrition education across the country and issues of food fortification so that we put the missing nutrients into our food. The first 1 000 days of a child are important because any damage is irreversible. As a ministry, we should have programmes to educate the nation on health issues,” Kamwende said.
Vulindlela Ndlovu of the Association of Health Funders of Zimbabwe said there was need to ensure all stakeholders were invited to planning sessions of the health budget. He said there was need to broaden the Aids levy into a health fund that would also cover other diseases that were not funded by donors.