As the economy continues on a tailspin, the health delivery system is one of the biggest casualties.
According to human rights groups and activists, government hospitals have virtually become death traps as they do not have enough medication and staff.
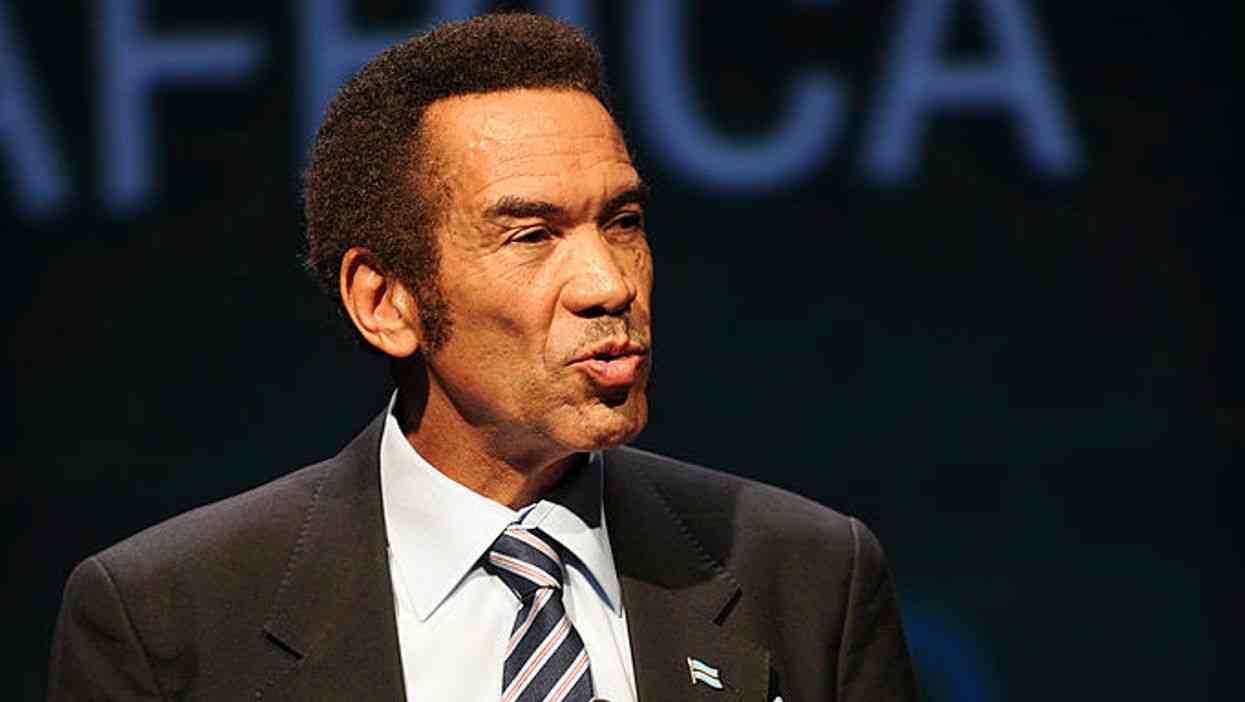
Health and Child Care minister David Parirenyatwa (DP) last week spoke to our senior reporter Xolisani Ncube (XN) about measures government is taking to revive the ailing health sector.
Below are excerpts of the interview:
XN: What is the current status of the health system in the country? Are we safe, considering the state of our economy?
DP: Let me start by saying we are safe and very sound although with numerous challenges. You will find that our health sector is far much better than the way it was. The most important aspect of a health delivery system is the human capital or workers. Medicine is the second most important thing. The third one is infrastructure, the buildings, the clinics, equipment in the hospital and so on and the fourth is communication, which is the telephones, the ambulances and a reliable transport system and the most common and critical is the financing.
So for us in Zimbabwe, we have lobbied as a ministry that we cannot continue to depend on donors for medicines and our government should look for means to deal with this. I am in the process of agreeing with the Reserve Bank of Zimbabwe governor (John Mangudya) and the Finance ministry to use Treasury Bills to get money so that we can have drugs in bulk and I think that will work because there is a serious shortage of essential drugs in the country. We are hoping that we can be able to use the Treasury Bills so that somebody can bring us these drugs en masse.
- Chamisa under fire over US$120K donation
- Mavhunga puts DeMbare into Chibuku quarterfinals
- Pension funds bet on Cabora Bassa oilfields
- Councils defy govt fire tender directive
Keep Reading
In health, the most important things are doctors, nurses and those other trained people. Now what we have is an establishment of the health sector which was put up in 1983; in other words, the establishment that we have now is an 1983 establishment, but our diseases have increased, the population has increased, hospital numbers have increased so we need an establishment that is going to cope with that increase, so we are asking the Treasury to put up the establishment. For example, our establishment for nurses is 11 600 and we want to put up that establishment by about 8 000 more so that we can cope with our vision.
But remember, we want 8 000 more nurses and we have 4 000 nurses that are trained, but are unemployed, so if we put up the establishment, we can absorb all these nurses and we need them because a lot of clinics are understaffed.
We want all specialists in all our provincial hospitals. If we have those specialists out there, there won’t be any need to refer all patients to Parirenyatwa or Harare Central because they will be catered for at these provincial hospitals.
We are going a step further. we are saying at every district hospital, there used to be only two doctors, but since last year we deployed three doctors at each district hospital with some having four, but we want them to be five in each particular district hospital so that one of the doctors is able to go round the clinics that feeds the district hospital.
XN: Which is the most dangerous disease in the country at the moment and what is government’s action to contain it?
DP: Our number one at this moment is HIV, with malaria and tuberculosis coming second and then you come to non-communicable diseases like diabetes, high blood pressure and you know, a lot of people you just hear they have had a stroke and it is because of high blood pressure.
We need to look at those. But critically, one which is growing most dangerous is cancer across the board. Cancer in men in terms of cancer of the prostate, and cancer in women in terms of cancer of the breast and cancer of the cervix. Those are the things that we need to fight.
You see, when we were fighting HIV, we were using three principles, which are prevention, prevention and prevention. For cancer, that is exactly what is needed. The structures that we had for HIV, we want to use them from the district levels down to the ward. We want to decentralise the fight against cancer.
XN: Previously, the fight against cancer has been funded by the donor community, where is government?
DP: Government is there and is playing its role. We have two centres that are meant for cancer treatment. We have one at Parirenyatwa and one in Bulawayo, where we have state-of-the-art machines. But that is not enough, we need to decentralise that more, but more importantly, is actually to prevent that more and to detect it early. We are also thinking of vaccination against cancer of the cervix in nine year olds. So that is the way to go, to prevent, prevent and prevent.
XN: There have been calls for the establishment of a cancer levy. What is your view on that?
PD: I don’t mind having levies for one disease I think we need to then say are our people ready to take these levies? Why don’t we put that together in one basket like this Aids Levy and also partly use it to fight cancer, can we not do that? I think we need to ook into that with actuarial people from the Finance ministry. I am not against that, but we need to look at that as a country.
XN: Let’s talk about HIV and new infections. How have we performed as a country in the fight against the pandemic?
DP: We have done extremely well; we have managed to reduce the prevalence rate from 29% to 14%, and it’s commendable. We are actually used as an example by many countries on how we fought it and still we are fighting it. Now our target is on the young people, those between the ages of 15 and 24. We have discovered that there is a high prevalence rate in that group. We are also targeting commercial sex workers and truck drivers. Our main strategy is to start educating these young people about prevention as a tool to fight HIV.
XN: We have read reports that you got $100 000 from the Premier Medical Aid Society (PSMAS) at a time when most doctors were not getting anything from the health insurer. What really happened?
DP: We have always had a good working relationship in general with medical aid societies, but remember I have been practising since 1984 and the medical aid business really started picking up in 1990. We have always had a relationship where sometimes the medical aids would not pay you on time and sometimes they take months to pay and this is exactly what happened.
During that time, I decided that my practices, in fact, it’s a practice that is being run by other doctors because I am here as a minister so in this particular case, PSMAS had not paid me for about five months, that is from around end of 2013 and I continued to lobby them that I wanted my money.
We calculated from our surgery that it was about $55 000, but they had to do reconciliation because you submit claims and some of them are rejected, some of the people are not on medical aid, so then you have to reconcile all those things.
But from our surgery, we calculated that it was $55 000. So when they had not paid me for those months, I had a lot of debts. I could not pay salaries properly and then I said, like normal practice, like it happens in other institutions where medical aid can actually advance you as a business, can you advance me money, so this is what happened.
They gave me $55 000 and then I asked for an advance. My surgery asked for $45 000. What is being said, that I was given an advance of $100 000, it is not true.
But they had to reconcile later on to know it was $45 000 not $55 000, so that was about March of 2014 and then the arrangement was that you will pay back from the claims that come to PSMAS from your patients.
So this thing was done in March, 2014. In May 2015, they started to deduct money from my dues, there was no stealing at all because this is an arrangement where you are paying everything. It’s like an overdraft, it’s a proper procedure and I was paying with some months as we were not getting anything from PSMAS.
When the noise started, I was advised to just pay the remainder in full, which is exactly what I did. You can check with PSMAS whether what I am saying is not true. They can give you a schedule of how I was paying.
XN: Some are saying you forged documents to prove that you paid?
DP: How can I forge? You can go to PSMAS and check, I can’t forge such a thing, to prove to who?
XN: There are allegations that you allowed PSMAS to collapse because some ministers including yourself were on the payroll of the insurer.
DP: No! Not at all! Remember, I am a practicing doctor. Well, I was a practising doctor. The relationship that I have with PSMAS is based on patients, nothing more. Why would I be on the payroll, for what because I was running my own surgery? Our relationship was purely business.
XN: There are reports that the HIV infection rate is very high in prisons, what is the ministry doing to deal with the problem?
DP: The background is that in prisons a research was done. A very solid research while in the general population we have talked about it, the prevalence is 14% in the general population, in prison it is 28%, you understand, the prevalence, and we are saying why?
And that is a question that has not been answered. We need another research to establish if these people come in already infected or do they get it inside? Now if they get it inside how is it happening? It means men are having sex with men.
That’s the controversy, but clearly, something is happening here, we can’t have 14% and 28% and not explain it somehow and we have said maybe sometimes it may be better to screen people as they come to prisons or maybe just routinely test them for HIV and see.
XN: But won’t that be interpreted as discrimination?
DP: I am saying this is the only research you can do to find out if they are getting it inside or if they come with it. How else do you find out? The only way to find out is to screen them when they come in.
XN: There are some MPs who are saying let’s distribute condoms to prisoners.
DP: We would look at people who are in prison as a programme. Again, we would not attribute blame on them, but we would recognise that one of the ways of preventing spreading HIV and Aids in prisons would probably be the use of condoms.
Now, how do you do that, a lot of research that we have done actually says the prisoners inside do not want condoms put in prisons because they are saying what is my wife saying outside, that I am now having condoms?
There are perceptions that the public will now say that we are accepting it that you are doing something in prisons, but from our point of view, condoms could be put in prisons discreetly because it has been done in certain countries and we want to know if that is working well in Lesotho as they do that. they put condoms in prisons.
It’s the thing that we must look at. We can talk about prevention but there is a lot of crowds in prisons . . . so yes, that can happen, so it’s realistic.
XN: Some are suggesting that prisoners must be allowed to enjoy conjugal rights.
PD: From a health perspective, it’s a good thing to have conjugal rights, conjugal privileges in prisons, probably once or twice a week or whatever, or once a month.
But it needs for the prison to build up private rooms, all that infrastructure is needed, are they able to afford it? Conjugal rights how? Will these people be allowed to go home? That is a security risk so you will need to build something there and lock them in or something like that, so all those imponderables are there.